Emerging research suggests that a class of diabetes medications known as glucagon‑like peptide‑1 receptor agonists (GLP‑1 RAs) could significantly reduce complications after partial nephrectomy for renal cell carcinoma (RCC) , a common kidney cancer surgery.
This potential GLP‑1 RA benefitafter kidney cancer surgery has captured the attention of clinicians and patients alike because it opens the door to using established metabolic drugs to support recovery from cancer surgery.
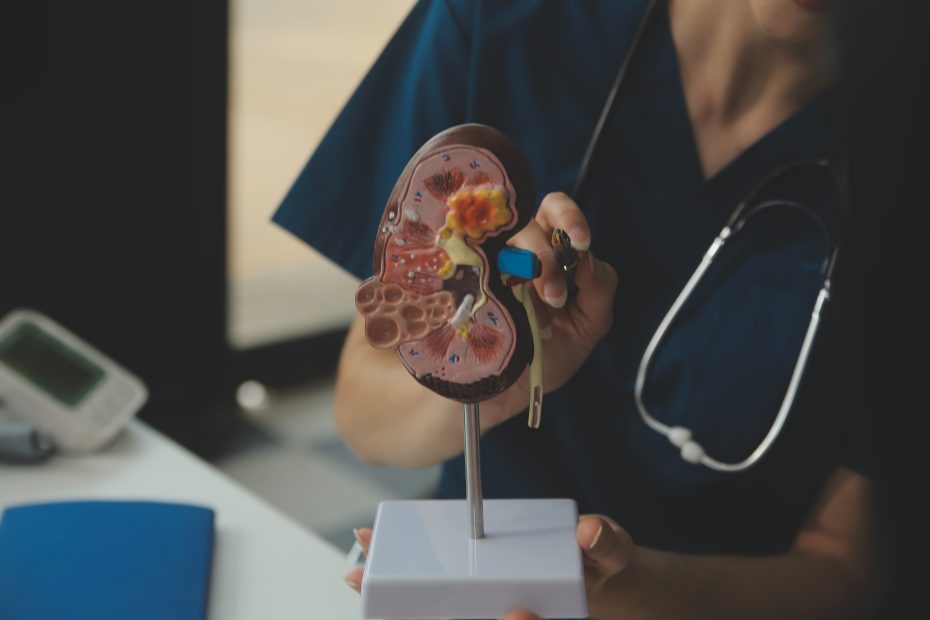
Partial nephrectomy is a procedure that removes only the tumour from the kidney while preserving as much healthy tissue as possible. It is the recommended approach for early‑stage RCC because it balances cancer control with preservation of renal function.However, like many major operations, it carries risks of complications , including bleeding, infection, acute kidney injury and hospital readmission , particularly within the first 90 days after surgery.
A recent observational analysis, reported by both Oncology Nurse Advisor and Renal & Urology News, found that patients who were taking GLP‑1 receptor agonists at the time of surgery had significantly lower rates of specific post‑operative complications than those who were not on these medications.
According to the reports, GLP‑1 RA treatment was linked with reduced odds of adverse outcomes within 90 days of partial nephrectomy , including fewer cases of acute kidney injury, cardiac issues and hospital readmissions. Although this analysis does not establish cause and effect, the associations are consistent enough to draw clinical interest.
These findings are particularly interesting because GLP‑1 RAs are widely prescribed and worldwide for type 2 diabetes and obesity due to their proven metabolic benefits. The class includes medications such as semaglutide and liraglutide, which are known to help control blood glucose and support weight loss. Their metabolic effects also include improved cardiovascular outcomes and, increasingly, positive impacts on kidney health.
The mechanisms behind the potential GLP‑1 RA benefit after kidney cancer surgery are not fully understood, but researchers think that the renal and anti‑inflammatory effects of these drugs could contribute. GLP‑1 RAs are linked with improved kidney blood flow, reduced oxidative stress, and slower decline in kidney function in people with chronic metabolic conditions, effects that may support recovery after major surgery.
Large meta‑analyses also show broader kidney benefits with GLP‑1 receptor agonists. For example, pooled data from multiple randomised controlled trials indicate these drugs can reduce the risk of clinically meaningful kidney outcomes, including slower progression of kidney disease and lower rates of kidney failure, particularly in people with type 2 diabetes.
That said, it remains unclear whether these mechanisms translate directly to the surgical setting. The current evidence for post‑surgical benefit comes from retrospective data, and there are important limitations: patients on GLP‑1 RAs may differ systematically from those not on these drugs in ways that also influence recovery outcomes.
The wider scientific literature shows that GLP‑1 RAs are increasingly recognised for organ‑protective properties beyond blood sugar control. Meta‑analyses reveal reductions in major adverse cardiovascular events and kidney disease progression in diabetes populations, and there’s growing exploration of effects in non‑diabetic groups as well.
Indeed, regulatory agencies such as the US Food and Drug Administration (FDA) recently approved a GLP‑1 RA , semaglutide , to reduce the risk of kidney failure and cardiovascular death in people with type 2 diabetes and chronic kidney disease, highlighting expanding therapeutic uses.
However, experts emphasise that the data linking GLP‑1 RAs to better outcomes after kidney cancer surgery are still preliminary, and should not prompt patients to start or change medications without medical advice. Larger, prospective clinical trials are needed to determine whether GLP‑1 RAs can truly reduce surgical risk and pinpoint which patients benefit most.
For clinicians, these findings may inform discussions in multidisciplinary teams about peri‑operative care, especially in patients already taking GLP‑1 RAs for diabetes or obesity. While not yet part of surgical guidelines, the potential GLP‑1 RA benefit after kidney cancer surgery encourages further research into how metabolic interventions intersect with oncological outcomes.
Patients should talk openly with their healthcare teams before making changes to their medication. As with all observational research, there is a risk of unmeasured confounding , meaning that the associations observed may not be directly caused by the drugs themselves.
Sources:
- GLP‑1 RA Use May Reduce the Chances of RCC Partial Nephrectomy Complications, Renal & Urology News – https://www.renalandurologynews.com/reports/renal-cell-carcinoma-rcc-glp1-ra-use-reduce-partial-nephrectomy-complications/ renalandurologynews.com
- GLP‑1 RA Use May Reduce the Chances of RCC Partial Nephrectomy Complications, Oncology Nurse Advisor (summary) – https://www.oncologynurseadvisor.com/news/renal-cell-carcinoma-rcc-glp1-ra-use-reduce-partial-nephrectomy-complications/ oncologynurseadvisor.com
- GLP‑1 receptor agonists’ renal benefits and mechanisms – meta‑analysis and clinical data Springer Link
- Meta‑analysis of GLP‑1 RA effects on kidney outcomes and cardiovascular risk PubMed